A recent study published by life sciences company Grace Health & Wellness aims to raise awareness on the possibility of using medical cannabis and psychedelics to propel traditional pharmaceuticals. The study presented positive outcomes in a case of advanced breast cancer, constituting the first-ever scientific report of this kind and gripping evidence of their healing potential.
Nicole Di Monda was diagnosed with stage IV metastatic breast cancer in September 2018. While undergoing commonly prescribed treatment, she decided to incorporate psilocybin microdoses and whole-plant (THC+CBD) edible cannabis formulations in her therapy, assisted by her husband, an endocannabinologist Jaime Brambila.
The alternative medicine improved the effectiveness of her treatments, as results suggest a link between the use of cannabis and psychedelics with a reduced level of body inflammation, improved tumor management, and better mental health overall.
Furthermore, the timeline data from the patient’s treatment suggests that stopping these adjunct therapies “coincided with a destabilizing of the patient’s condition and a re-emergence of rapidly multiplying cancer cells within her body,” after which Nicole decided to reintroduce the psychedelic and cannabinoid substances to her treatment, which consequently improved her health.
Nicole Di Monda’s Compelling Testimony
“Cannabis and psilocybin saved my life as I was able to eat, sleep and function, and my nausea became almost non-existent. The beneficial effects gave me a way to recover with dignity and empowerment, which are everything. Understanding my options was the game changer because I was no longer a slave to my disease. Plant medicines gave me hope.”
Brambila, co-founder and CSO of Grace Health & Wellness, said he hoped that future breast cancer patients will complement their pharmaceuticals with cannabis medicine. To that end, the organization is now preparing to undergo preclinical and clinical trials in the US to further study the cannabis’ potential in treating breast cancer and potentially “pave the way for wider use.”
Brambila added that patients are eager for approval. “We see the therapeutic potential for patients deciding to safely explore by themselves and sometimes in partnership with their physicians.” Brambila concluded that the relevance of Di Monda’s case study is in that it exemplifies a strategic polypharmaceutical approach to cancer. “Cannabis is the quintessential example of a multipurpose integrative tool that stimulates a range of physiological functions,” he affirmed.
In London, the Imperial College Medical Cannabis Research Group is already involved in studying how individual cannabinoids may have anti-neoplastic effects, therefore supporting cancer treatments.
With respect to Nicole’s particular case, senior clinical lecturer at Imperial College London Dr. Mikael Sodergran stated that while her response to combined treatment was “fantastic,” it’s not possible to “draw any conclusions regarding the efficacy of cannabis-based medicinal products for the treatment of breast cancer based on this report.”
Nonetheless, he acknowledged that current evidence “is promising.”
Imperial College of London’s Dr. Rayyan Zafar added that while caution is “absolutely key,” scientists are optimistic, as clinical trials in late-stage cancer could help get these therapeutics approved as legal therapies “and it could well be a revolution in cancer treatment.”
Dr. Dustin Sulak, one of Di Monda’s physicians and a specialist in osteopathic and integrative medicine and medical cannabis, believes the use of cannabis and psilocybin in cancer treatments is “invaluable,” and that “witnessing their impact has been profound.”
“They can improve the patient’s quality of life, relieve pain, depression, and anxiety while promoting psychological adaptation to a challenging diagnosis and prognosis. They may also enhance our innate anti-cancer mechanisms and work additively or synergistically with other treatments.” Dr. Sulak further explained.
His clinical experience has shown him that “all patients with cancer can significantly benefit in some way from the appropriate use of cannabis and psilocybin,” and he believes that the future standard of care will include them.
Sulak explained how the science behind it might work. “This therapeutic effect has potential in interventions for chronic disease. The anti-neoplastic effects of cannabinoids are stimulated when these compounds synergistically activate chemical receptors. The endocannabinoid system, discovered in the nineties, creates homeostatic balance.”
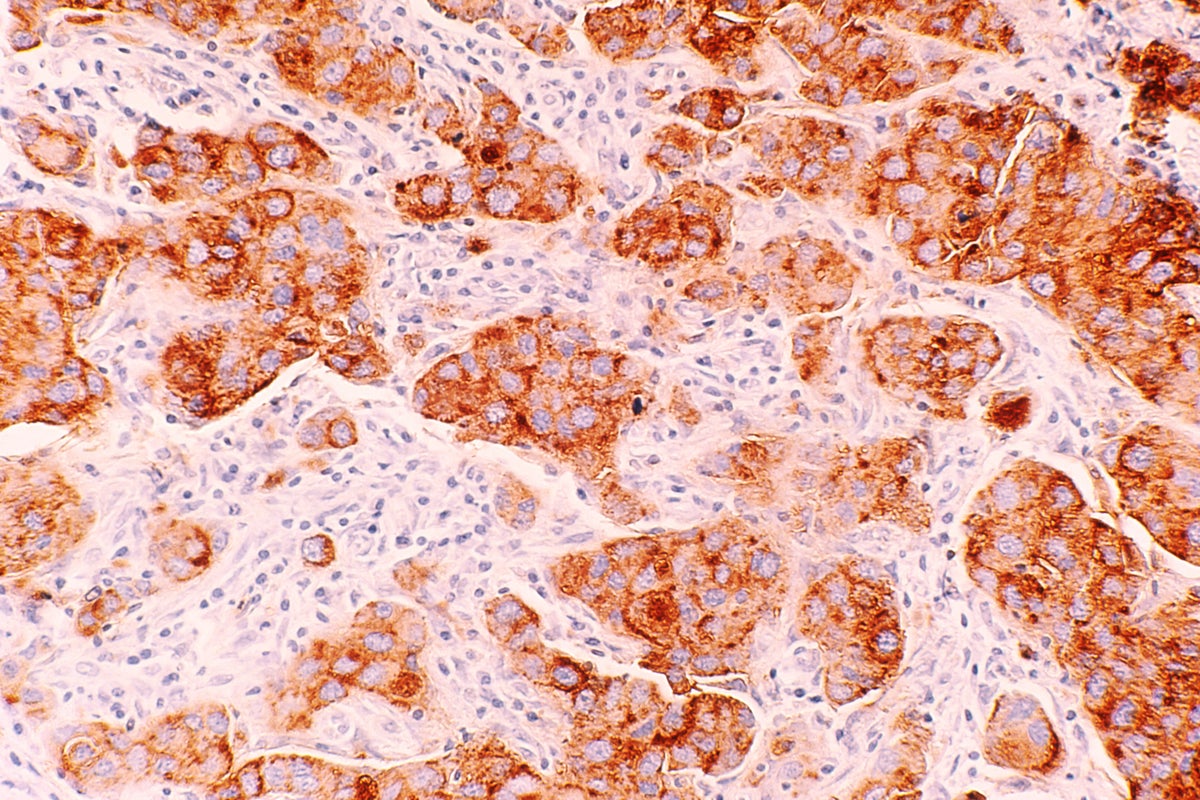
Photo by National Cancer Institute on Unsplash
Image and article originally from www.benzinga.com. Read the original article here.